Interface Fluid Syndrome After LASIK
Interface fluid syndrome may occur secondary to steroid-induced elevation of intraocular pressure (IOP) after LASIK. Interface fluid syndrome after LASIK is sometimes misdiagnosed as diffuse lamellar keratitis (DLK) and treated improperly with topical steriods which may lead to worsening of the condition. High IOP may cause damage to the optic nerve, leading to vision loss.
Problems from Lasik? File a MedWatch report with the FDA online. Alternatively, you may call FDA at 1-800-FDA-1088 to report by telephone, download the paper form and either fax it to 1-800-FDA-0178 or mail it to the address shown at the bottom of page 3, or download the MedWatcher Mobile App for reporting LASIK problems to the FDA using a smart phone or tablet. Read a sample of LASIK injury reports currently on file with the FDA.
Patients with LASIK complications are invited to join the discussion on FaceBook
Below are abstracts of peer-reviewed journal articles which report interface fluid syndrome after LASIK.
Interface Fluid Syndrome in Routine Cataract Surgery 10 Years After Laser In Situ Keratomileusis.
Cornea. 2012 Feb 29.
Ortega-Usobiaga J, Martin-Reyes C, Llovet-Osuna F, Damas-Mateache B, Baviera-Sabater J.
Clínica Baviera, Instituto Oftalmológico Europeo, Madrid, Spain.
Abstract
PURPOSE: Interface fluid syndrome is an unusual complication after laser in situ keratomileusis (LASIK). We present a case of interface fluid syndrome after cataract surgery in a patient who had previous LASIK surgery.
METHODS: A 62-year-old man underwent routine cataract surgery on the left eye 10 years after LASIK on both eyes. The day after surgery, the intraocular pressure (IOP) was 21 mm Hg and a pocket of fluid was present in the interface LASIK wound. The patient was treated with 0.50% timolol eye drops twice daily.
RESULTS: The problem resolved within 1.5 months. Two months later, the patient underwent routine cataract surgery of the right eye. The next day, the IOP was 11 mm Hg and LASIK interface fluid was present. The patient was treated with 0.5% timolol eye drops twice daily. Two months after the surgery, the problem had completely resolved.
CONCLUSIONS: Ocular hypertension and traumatic endothelial cell damage could have been the causes of the syndrome. Although the IOP was not very high, previous LASIK could have led us to underestimate the IOP.
Delayed-onset interface fluid syndrome after laser in situ keratomileusis secondary to combined cataract and vitreoretinal surgery.
J Cataract Refract Surg. 2011 Dec 24.
Han SB, Woo SJ, Hyon JY.
Abstract
A 40-year-old man with a history of laser in situ keratomileusis (LASIK) 13 years earlier had combined cataract extraction and vitreoretinal surgery due to rhegmatogenous retinal detachment and posterior subcapsular cataract. Two weeks postoperatively, he complained of painless visual blurring. Diffuse interface haze was observed, and antiinflammatory treatment including topical steroid and cyclosporine was started. One week later, visual blurring had not improved and intraocular pressure was 27 mm Hg. Interface haze, fluid collection, and flap edema were observed and confirmed by spectral-domain anterior segment optical coherence tomography. After discontinuation of the steroid and addition of IOP-lowering medication, visual acuity and interface fluid collection and haze improved. This case illustrates that interface fluid syndrome can develop more than 10 years after LASIK, triggered by ocular hypertension and inflammation after intraocular surgery.
Elevated Intraocular Pressure-Induced Interlamellar Stromal Keratitis Occurring 9 Years After Laser In Situ Keratomileusis.
Cornea. 2011 Sep 20.
Lee V, Sulewski ME, Zaidi A, Nichols CW, Bunya VY.
Abstract
Elevated intraocular pressure-induced interlamellar stromal keratitis (PISK) is an entity of interface haze usually occurring weeks to months after laser in situ keratomileusis (LASIK) that is associated with elevated intraocular pressures and worsening with steroid treatment. There is evidence that this interface haze is the result of abnormal fluid dynamics that occur in the cornea after LASIK. We present a case of pressure-induced interlamellar stromal keratitis occurring 9 years after LASIK in the setting of anterior uveitis. This case emphasizes the importance of considering such diagnoses as pressure-induced interlamellar stromal keratitis in the differential diagnosis when presented with a patient with corneal haze and a history of LASIK.
Interface Corneal Edema Secondary to Steroid-induced Elevation of Intraocular Pressure Simulating Diffuse Lamellar Keratitis
Journal of Refractive Surgery Vol. 22 No. 5 May 2006
Ahmed Galal, MD, PhD; Alberto Artola, MD, PhD; Jose Belda, MD, PhD; Jose Rodriguez-Prats, MD, PhD; Pascual Claramonte, MD, PhD; Antonio Sánchez, MD, PhD; Oscar Ruiz-Moreno, MD, PhD; Jesús Merayo, MD, PhD; Jorge Alió, MD, PhD
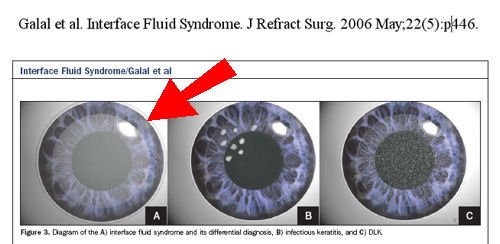
PURPOSE: To describe interface corneal edema secondary to steroid-induced elevation of intraocular pressure (IOP) following LASIK.
METHODS: Retrospective observational case series. Diffuse interface edema secondary to steroid-induced elevation of IOP was observed after LASIK simulating diffuse lamellar keratitis (DLK) in 13 eyes. Mean patient age was 31.4±5.3 years. Patients were divided into two groups according to provisional misdiagnosis: DLK group (group 1) comprised 11 eyes and infection group (group 2) comprised 2 eyes (microbial keratitis). Mean follow-up was 8.1±0.5 weeks.
RESULTS: In the DLK group, typical diffuse haze was confined to the interface and extended to the visual axis, impairing vision in all eyes. Provisional diagnosis was late-onset DLK and topical steroids were started. Repeat examination showed elevated IOP as measured at the corneal center and periphery using applanation tonometry (mean 19.1 mmHg and 39.5 mmHg, respectively), causing interface edema with evident interface fluid pockets. Steroids were stopped and topical anti-glaucoma therapy was started. The interface edema decreased and at the end of follow-up the corneal transparency was restored and IOP dropped to normal values. The infection group demonstrated a microbial keratitis-like reaction and underwent flap lifting and interface wound debridement and biopsy with administration of fortified antibiotics and steroids. After elevated IOP was detected, steroids and antibiotics were stopped and topical anti-glaucoma therapy was started, resulting in the resolution of the interface edema.
CONCLUSIONS: Interface fluid syndrome secondary to steroid-induced elevation of IOP might develop in steroid responders after LASIK with a misleading clinical picture simulating DLK or infectious keratitis. Management includes stopping topical steroids and starting topical anti-glaucoma therapy.
Pressure-Induced Interlamellar Stromal Keratitis After Laser In Situ Keratomileusis.
Cornea. 2011 Apr 20.
Tourtas T, Kopsachilis N, Meiller R, Kruse FE, Cursiefen C.
PURPOSE: To describe a patient with interlamellar stromal keratitis induced by increased intraocular pressure (IOP) [Pressure-induced interlamellar stromal keratitis (PISK)] after laser in situ keratomileusis (LASIK) surgery.
METHODS: Case report and review of the literature.
RESULTS: We report a case of interlamellar stromal keratitis induced by increased IOP after LASIK surgery. A 42-year-old man presented with persistent interface haze after uneventful LASIK. The patient described onset of decreased visual acuity after the first 2 postoperative weeks, failed to improve with high-dose topical steroid drops, and had significantly elevated IOP values up to 48 mm Hg. IOP was resistant to maximal topical antiglaucomatous therapy. The patient showed both improvement in visual acuity and decrease in interface haze after discontinuation of topical steroids and lowering of IOP by both topical and systemic treatment. Slit-lamp optical coherence tomography ruled out a fluid accumulation in the interface.
CONCLUSIONS: PISK appears clinically almost identical to diffuse lamellar keratitis after LASIK. It is important to measure the IOP and be suspicious when a diffuse interface haze occurs after the first postoperative week, is resistant to or even exacerbates in response to an increase in topical steroid treatment, and is not associated with other causative events. Slit-lamp optical coherence tomography is a valuable tool that allows differentiation between space-occupying interface fluid collection and non-space-occupying interface fluid collection to avoid falsely low or normal IOP measurements in PISK.
J Refract Surg. 2009 Feb;25(2):235-9.
Steroid-induced interface fluid syndrome after LASIK.
Moya Calleja T, Iribarne Ferrer Y, Sanz Jorge A, Sedó Fernandez S.
PURPOSE: To report ocular manifestations of eyes that developed interface fluid syndrome secondary to steroid-induced elevation of intraocular pressure (IOP) after LASIK. The patients presented with similiar characteristics of diffuse lamellar keratitis (DLK).
METHODS: Retrospective evaluation of four eyes of three patients with loss of vision, fluid in the lamellar interface, and IOP and topographic changes due to prolonged treatment with topical corticosteroids after LASIK.
RESULTS: Slit-lamp microscopy revealed an optically clear fluid-filled space between the flap and stromal bed. After early diagnosis, treatment with topical corticosteroids was stopped, resulting in quick and progressive cessation of symptoms.
CONCLUSIONS: A steroid-induced rise in IOP after LASIK can cause transudation of aqueous fluid across the endothelium that collects in the flap interface. It is important to make an early differential diagnosis of interface fluid syndrome in DLK-suspected cases, as continued treatment with corticosteroids can produce serious visual loss.
Am J Ophthalmol. 2005 Jun;139(6):1137-9.
Uveitis-associated flap edema and lamellar interface fluid collection after LASIK.
McLeod SD, Mather R, Hwang DG, Margolis TP.
PURPOSE: To report two cases of corneal pathology associated with anterior uveitis after laser in situ keratomileusis (LASIK).
DESIGN: Observational case report.
METHODS: A 47-year-old man and a 50-year-old woman who experienced vision loss and corneal changes associated with acute anterior uveitis after LASIK were examined.
RESULTS: The 47-year-old man, who had undergone LASIK for low myopia developed an interlamellar fluid pocket at the level of the flap interface, whereas the 50-year-old woman, who underwent LASIK for hyperopia, developed marked flap edema without interface fluid collection.
CONCLUSIONS: These two cases demonstrated acute corneal fluid accumulation associated with episodes of acute anterior uveitis in eyes that had undergone LASIK. Uveitis should be considered a risk factor for vision threatening corneal complications after LASIK.
Ophthalmology. 2002 Apr;109(4):659-65.
Steroid-induced glaucoma after laser in situ keratomileusis associated with interface fluid.
Hamilton DR, Manche EE, Rich LF, Maloney RK.
PURPOSE: To report the ocular manifestations and clinical course of eyes developing interface fluid after laser in situ keratomileusis (LASIK) surgery from a steroid-induced rise in intraocular pressure.
DESIGN: Retrospective, noncomparative interventional case series.
PARTICIPANTS/INTERVENTION: We examined six eyes of four patients who had diffuse lamellar keratitis develop after uneventful myopic LASIK surgery and were treated with topical corticosteroids.
PRINCIPAL OUTCOME MEASURE: Slit-lamp findings, intraocular pressure measurements, and visual field loss.
RESULTS: All eyes had a pocket of fluid develop in the lamellar interface between the flap and the stromal bed associated with a corticosteroid-induced rise in intraocular pressure. However, because of the interface fluid, intraocular pressure was normal or low by central corneal Goldmann applanation tonometry in all eyes. The elevated intraocular pressure was diagnosed by peripheral measurement in several cases after months of elevated pressure. All six eyes had visual field defects develop. Three eyes of two patients had severe glaucomatous optic neuropathy and decreased visual acuity develop as a result of undiagnosed steroid-induced elevated intraocular pressure.
CONCLUSIONS: A steroid-induced rise in intraocular pressure after LASIK can cause transudation of aqueous fluid across the endothelium that collects in the flap interface. The interface fluid leads to inaccurately low central applanation tonometry measurements that obscure the diagnosis of steroid-induced glaucoma. Serious visual loss may result.
Ophthalmic Surg Lasers Imaging. 2008 Jul-Aug;39(4 Suppl):S80-2.
High-resolution imaging of complicated LASIK flap interface fluid syndrome.
Ramos JL, Zhou S, Yo C, Tang M, Huang D.
The authors report a case of post-LASIK interface fluid syndrome that led to epithelial ingrowth, a sequelae that had not been reported to date. The interface fluid was caused by steroid-induced ocular hypertension. On post-LASIK day 49, the interface fluid, epithelial ingrowth, and noncellular reflective deposits were visualized by confocal microscopy and high-resolution Fourier-domain optical coherence tomography. No inflammatory cells or infectious organisms were seen. These high-resolution imaging technologies were useful in the noninvasive evaluation of the location and nature of flap interface pathologies at the microstructural level.
Disclaimer: The information contained on this web site is presented for the purpose of warning people about LASIK complications prior to surgery. LASIK patients experiencing problems should seek the advice of a physician.